Another health issue I have to come to terms with? This is seriously impacting the quality of my “Retired Tranquil in Thailand” life. A new medical condition has occurred recently (Sept/Oct 2025) with the onset of disturbing skin blisters breaking out on my face, scalp, front, and back of my torso. Visits to three different dermatologists over a few months failed to diagnose the problem or prescribe a course of treatment. In December, I had had enough (!) and was really concerned that there was more to what was going on. I felt unwell, not able to sleep properly, and felt things were more serious.
Khon Khan – December Consult
This led us to an appointment with a dermatologist at Khon Kaen University (Srinagarind) Hospital before Christmas 2025 for a diagnosis and medical intervention. It is a 4-hour drive there for an evening appointment, and we stay overnight. We did try to enjoy the trip, given the circumstances, with some subdued shopping & food delights.
The doctor was pleasant, spoke good English, and after an examination and discussion, he determined that a further skin biopsy was required. A series of lab tests was ordered, but he informed me that the results would likely be one of two suspected diseases. One disease was very concerning, and he hoped it was not that. Given the Thai year-end holiday period, the next appointment for the results was not until 9 January. That was a worry for me, but I was prescribed various lotions to apply in the meantime to assist in controlling symptoms somewhat.

Khon Khan – January Diagnosis
Anxiety was on my face at our appointment, where it was revealed that lab work & further confirmation testing resulted in a diagnosis of: Superficial pemphigus, or pemphigus foliaceus (PF), which apparently is a rare autoimmune skin disease in which the body attacks its own skin cells, causing fragile, itchy, crusty blisters and erosions, typically on the scalp, face, and chest. It usually has a better prognosis than deeper forms and is often managed with steroids or other immunosuppressants.
I am told there is no cure for autoimmune disease, but a drug-risk management regimen can help control the symptoms and potentially suppress the problem for a more enjoyable life. Only time will tell. For more specific information on the disease, refer to the Annex at the bottom of this post. The causes of this disease are not certain; however, based on what is known about it, I believe that significant UV exposure during our house build, along with considerable antibiotic use more recently (while dealing with urology matters), might have been the trigger for me.
For now, I am on 30 mg a day of prednisone & vitamin tablets along with steroid creams for application to blisters daily and a moisturiser on my troubled areas. Going forward, the doctor has indicated that I may need to have an annual infusion of rituximab (a targeted therapy monoclonal antibody), requiring a one-day admission to the hospital. This drug avoids the long-term use of steroids and risky side effects. I will need regular blood tests & Dr visits to manage the risks associated with the use of steroids longer term, as well as other side effects from potential infections that the body can not fight due to steroid use.
Steroids (corticosteroids) used for autoimmune disease, while highly effective for suppressing inflammation, carry risks of significant side effects, particularly with long-term use. I was informed that prednisone can cause an increase in appetite and weight gain, along with fluid retention, increased infection risk, bone thinning, high blood sugar, hypertension, insomnia, mood changes and skin thinning- what a list of disadvantages, to get better! So far, I have managed to lose 6 kg, and for fluid retention, that is currently no issue. I have also been advised to stay out of the sun when possible or cover up extensively (if going out can not be avoided). I am apparently susceptible to getting infections easily with the medication. I have been asked to stay away from crowds and wear a mask in unavoidable situations with groups of people.
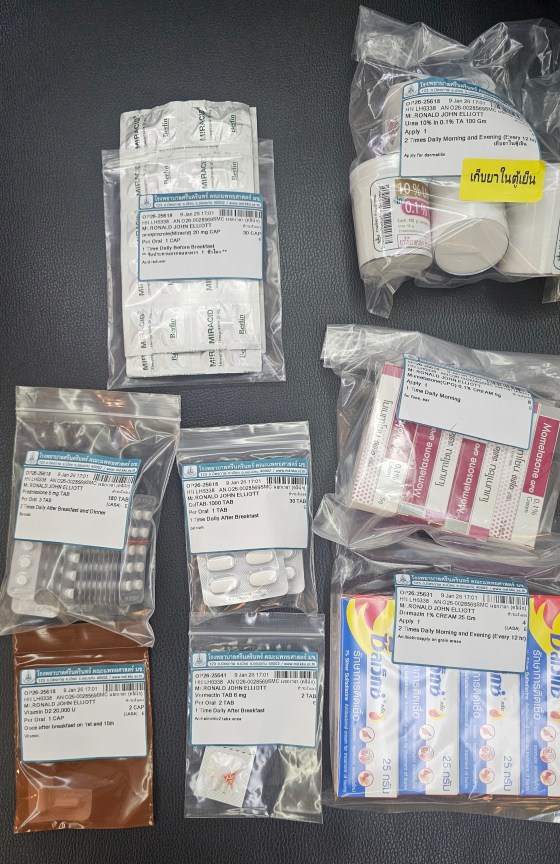
Impacts on Life – so I am trying to stay out of the intense UV sun of Thailand during the day. I can get out in the garden only early morning or after about 4:40 in the afternoon. We stay home much of the time, as I don’t want to risk infections from other people. We have increased our home cooking considerably; that is a good thing. My medication regimen is twice a day after meals. Ace is doing most of the garden chores these days. I am relegated to our back porch in the mornings for breakfast and doing some light housework. Sleeping at night can be a chore, often waking up and having difficulty going back to sleep. I am bothered by the blistering, itchy, etc. I am trying to take it all in my stride, & not get upset with the symptoms and side-effects.
As of the end of January 2026, skin blistering appears to be reduced and may be improving slightly after a few weeks on the medication. In reality, there is a long way to go. I take joy in small improvements, trying to be relaxed and accepting that life is full of changes & challenges to be met and tackled.
The next medical appointment to check on my progress with the hospital is in early February 2026. I will be able to update my diagnosis after that visit. Other than this mess, it’s all good. Wish me luck in early February.
Khon Khan – February 2026 Consult – TBA
Annex – Further Disease Information – Pemphigus Foliaceus (PF)
Pemphigus foliaceus cannot currently be cured, but it is highly manageable and often goes into long-term remission with appropriate treatment, allowing patients to live a normal life. Treatment, usually involving steroids and immunosuppressants, aims to control symptoms, heal skin lesions, and prevent flares, although long-term medication management is often necessary.
Key aspects of managing Pemphiqus Foliaceus:
Treatment Goal – the main objective is to reduce antibody production, clear blisters and achieve remission.
Medication – Corticosteroids: are commonly used (e.g., prednisone) to quickly bring the disease under control, often used as a first-line therapy. Immunosuppressants: medication is used to manage the condition and reduce dependency on steroids. Biologics: Rituximab is frequently used to target and deplete the B-cells responsible for producing the antibodies that cause the disease.
Topical Treatments – Creams or ointments (steroids or immunosuppressants) are used for localize, milder cases.
Remission: Many patients can eventually reduce or stop medication, but regular follow-ups with a dermatologist are necessary because flares can occur.
Prognosis: While chronic, the disease rarely affects life expectancy, and most patients can live without significant pain or active blisters once the disease is controlled. I will need to work with my dermatologist for a tailored long-term management plan.
Key Characteristics of this disease:
- Autoimmune: The immune system mistakenly creates antibodies that target proteins holding skin cells together, causing them to separate.
- Superficial Blisters: Blisters form high in the epidermis, leading to superficial, easily broken blisters, scales, and crusts rather than deep, painful sores.
- Common Sites: Starts in areas rich in sebaceous glands like the scalp, face (especially nose, ears), and upper back/chest.
- No Mucosal Involvement: A key differentiator from other pemphigus types; mouth sores are usually absent.
Causes and Triggers
Superficial pemphigus occurs when the immune system mistakenly attacks a protein that holds skin cells together in the upper epidermis. Medications: Certain drugs can induce drug-induced pemphigus. Common triggers include thiol-containing drugs, like penicillamine, as well as some antibiotics and anticonvulsants. Environment: UV exposure (sunlight) can worsen or provoke lesions.
Diagnosis and Treatment
A definitive diagnosis required a skin biopsy andimmunofluorescence to detect antibody deposits in the skin. Treatment options include: (1) Corticosteroids: Topical creams & oral prednisolone for more extensive disease. (2) Immunosuppressants: Drugs like azathioprine or rituximab may be used to reduce steroid dependency.
Taking systemic steroids (such as prednisone) is the conventional, first-line treatment for pemphigus foliaceus (PF) because they rapidly reduce inflammation and control the autoimmune attack on the skin. However, because PF often requires high doses and long-term treatment, the side effects can be severe, debilitating, and sometimes life-threatening, such as: (1) High Risk of Infections and Sepsis, (2) Metabolic and Cardiovascular Complications, (3) Musculoskeletal Degradation, (4) Psychological and Cognitive Effects, (5) Other Long-Term Effects
Managing the Risks
To minimize these side effects, physicians often: Taper Dosage: Start with a high dose to control the disease, then slowly reduce it to the lowest effective dose. Use Steroid-Sparing Agents: Introduce immunosuppressants like rituximab, early in treatment to reduce the reliance on long-term steroids. Provide Supplements: Prescribe calcium and vitamin D to protect bone health.
Because of these risks, the current consensus & recommended by my Doctor is to use steroid-sparing agents like rituximab as a first-line therapy to avoid long-term steroid toxicity. But that can be costly at around 20,000 THB an infusion. Time will tell if it is needed.
